There is now a way to strategically treat cancer because of the usage of not only the microenvironment of cancer, but also an in-vitro cancer model that simulates blood and lymphatic vessels, the main metastatic pathways. In the future, personalized cancer treatments will be possible by engineering a cancer model with cells from patients.
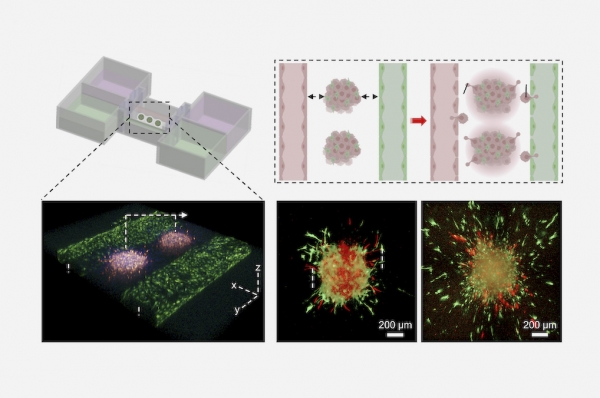
Professor Cho Dong-woo of the Department of Mechanical Engineering, Cho Won-woo and Ahn Min-jun of the integrated course, and Prof. Kim Byung-soo of the Department of Biomedical Convergence Engineering of Pusan National University produced a metastatic melanoma model using in-bath three-dimensional bioprinting technology. This model was made by printing cancer spheroids , which mimics the characteristics of metastatic melanoma, between artificial blood and lymphatic vessel pairs.
Earlier, the research team developed a technology to bioprint cancer spheroids inside the bioink bath. Using this technology, various sizes of cancer spheroids were produced with a biomimetic blood vessel. However, the original in-vitro cancer model did not include lymphatic vessels that are channels through which immune cells circulate and affect drug resistance.
Therefore, the research team was the first to produce a metastatic cancer model in which cancer spheroids, a blood vessel, and a lymphatic vessel coexist through in-bath bioprinting technology. As a result of the study, the hallmark events of metastatic melanoma such as local invasion and metastasis of cancer cells, and drug resistance by stromal cells were observed in the developed model.
Cancer can be treated more effectively by using an in-vitro cancer model. The progression of cancer and the effectiveness of treatments, which are different for each patient, can be confirmed outside the body in advance, reducing the burden on patients for chemotherapy. It is also expected that applying immune cells to the developed cancer model will allow us to observe the interaction between cancer cells and immune cells that actually occur in cancer and the resulting immune response.
Meanwhile, the study, recently published in the international journal, Advanced Science, was conducted with the support of the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT).


